- Visibility 193 Views
- Downloads 22 Downloads
- Permissions
- DOI 10.18231/j.ijpp.2022.029
-
CrossMark
- Citation
Right selection of oral anticoagulation for stroke prevention in atrial fibrillation
- Author Details:
-
Abhijit Anil Trailokya *
-
Debanu Ghosh Roy
-
Prafulla Kerkar
-
Shahid Merchant
-
Rajeev Sethi
-
Rajiv Karnik
-
S. C. Manchanda
-
Sadanand Shetty
-
Uday Jadhav
-
Vinod Vijan
Abstract
Atrial fibrillation (AF) is considered as one of the most common cardiac arrhythmias worldwide and is always associated with a significantly increased risk of stroke and thromboembolism. VKAs (Warfarin & Acenocoumarol) are highly effective in reducing the risk of stroke in patients with AF, but bleeding issues & disutility sparked the development of direct oral anticoagulants (DOACs) or NOACs (Novel oral anticoagulants). These drugs, offer the convenience of once or twice daily dosing without the need for laboratory monitoring of coagulation activity (PT/ INR) or routine dose adjustment. Various clinical trials proved their non-inferiority to warfarin (VKA) in reducing the risk of stroke or systemic embolism, and each was associated with markedly lower rates of ICH than well-adjusted warfarin. Yet there are no direct head-to-head comparative trials for the efficacy & safety of NOACs. In this review we try to provide patient centric approach to assist Indian physicians in selecting right OAC therapy for SPAF with respect to best possible evidence and recommendations available worldwide.
Introduction
One of the commonest arrythmia in clinical practice is Atrial fibrillation (AF) and it is estimated that about 1% of the population suffer from AF worldwide.[1] AF could be of valvular origin, typically rheumatic heart disease, but the vast majority of cases are of nonvalvular etiology. The risk of stroke secondary to either permanent or paroxysmal AF is the same and, should be treated in the same manner from the perspective of thromboprophylaxis.[2] AF is responsible for 15% of ischemic strokes overall, and in elderly it rising up to 25%.[3] Thromboprophylaxis is critical for the prevention of strokes in patients with AF (SPAF). Until recently, vitamin K antagonists (VKAs; e.g. warfarin & Acenocoumarol) and aspirin have been widely used to manage the risk of ischemic stroke in patients with AF. The VKAs are highly effective in stroke prevention; for example, well-controlled warfarin treatment can reduce the risk of ischemic stroke and systemic embolism by up to two-thirds and is associated with a 26% relative risk reduction in all-cause mortality in patients with nonvalvular AF.[4]
About 60% of patients never get VKA, around half of patients who do get it stop taking it especially in the developing world, and of those who still take it only half are in therapeutic range. So, only a small percentage of patients are well treated.[5]
The use of warfarin and Acenocoumarol in clinical practice is challenging due to problems such as a narrow therapeutic index and unpredictable anticoagulant effects, drug-drug and drug-food interactions, all of which result in the need for regular laboratory monitoring (PT/INR). So there is need to develop an effective oral anticoagulant with reliable pharmacokinetic profile so can be taken as fixed daily dosage, regardless of patient’s age, weight, ethnicity or gender.
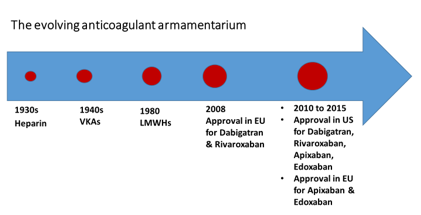
The non-VKA oral anticoagulants (NOACs like Dabigatran, Rivaroxaban, Apixaban) have changed the landscape of thromboprophylaxis for SPAF by offering physicians and patients the opportunity to use effective anticoagulants with predictable pharmacokinetic profiles, fewer drug– drug and drug–food interactions without the need for PT / INR monitoring and wide therapeutic windows.
Two classes of NOACs have been developed, and 3 drugs are currently licensed for use as anticoagulants in nonvalvular AF. The direct thrombin inhibitors (dabigatran) and the direct factor Xa inhibitors (rivaroxaban and apixaban).
In 2010, dabigatran etexilate, was approved for stroke prevention in non-valvular atrial fibrillation, marking the advent of a new age in anticoagulation. Prior to the development of dabigatran, efforts to develop a non-vitamin K antagonist (VKA) oral anticoagulant had been disappointing. The first such drug, ximelagatran, was never approved for use in the United States (US) after completion of phase 3 trials in VTE prevention and treatment due to hepatotoxicity.[6]
All four NOACs have been found to be noninferior to warfarin for the prevention of stroke and systemic embolism in large, international randomized control trials.
Till today, there is no evidence to demonstrate that any of the NOACs are superior to the others for the prevention of stroke in AF (SPAF). Indirect comparison between the NOACs is made tough by subtle differences between the patient cohorts enrolled in the randomized trials.[7]
|
Vitamin K Antagonist |
Non-vitamin K antagonists |
|
Acenocoumarin (Acenocoumarol) |
Direct thrombin inhibitor |
|
Warfarin |
Dabigatran |
|
|
Factor Xa inhibitor |
|
|
Rivaroxaban |
|
|
Apixaban |
|
Individual patient groups and characteristics |
OACs with characteristics beneficial to target group as per preference |
|
Asian Patients (Consider agents with reduced risk of ICH and major hemorrhage in Asian populations) |
Apixaban, Dabigatran |
|
Elderly patients (Consider comorbidities and agents with lower extracranial haemorrhage amongst elderly (age>75) |
Apixaban |
|
Poor patient, cost is the issue |
VKA (TTR should be ≥70%) |
|
Labile INR, inability to check INR regularly |
Dabigatran, Rivaroxaban, Apixaban |
|
Renal impairment (Consider agents with lower Haemorrhagic complications in moderate severe Renal impairment) |
Apixaban |
|
Previous GI haemorrhage / Patient with high risk of GI bleed |
Apixaban, Dabigatran 110 mg |
|
Need for reversal agent |
Dabigatran (Anti-dote available in India) |
|
High bleeding risk (HASBLED ≥3) (Consider agents with Lower incidence of extracranial haemorrhage) |
Apixaban, Dabigatran 110 mg |
|
Recurrent stroke despite well managed VKA |
Dabigatran 150 mg |
|
Preference for low pill burden (once daily formulation) |
Rivaroxaban |
|
Patient less likely to do well on VKA |
Any NOAC, but consider Patient characteristics when Choosing agent |
|
Patient with mechanical prostatic valves or moderate to severe mitral stenosis (for SPAF) |
VKAs |
|
Ischemic stroke while anti-coagulated on VKA (TTR more than 70 %) |
Dabigatran 150mg |
|
Molecule |
Dabigatran |
|
Rivaroxaban |
Apixaban |
|
Mode of action |
Direct thrombin inhibition (DTI) |
|
Factor Xa inhibition |
Factor Xa inhibition |
|
Dose |
110 mg BID |
150 mg BID |
20 mg once/day |
5 mg twice/day |
|
Study design |
Randomized, open label |
|
Randomized, double blind |
Randomized, double blind |
|
Number of patients |
18,113 |
|
14,264 |
18,201 |
|
Median follow up (years) |
2.0 |
|
1.9 |
1.8 |
|
Age (years) |
71.5 ± 8.7 (mean ± standard deviation) |
|
73 (65–78) median (interquartile range) |
70 (63–76) median (interquartile range) |
|
Mean CHADS2 score |
2.1 |
|
3.5 |
2.1 |
|
Mean warfarin TTR % |
64 |
|
55 |
62 |
|
Relative risk (95% CI) of stroke or systemic |
0.91 (0.74–1.11); p |
0.66 (0.53–0.82); |
0.88 (0.75–1.03); |
0.79 (0.66–0.95); |
|
Embolism versus warfarin |
< 0.001 for non- |
p < 0.001 for |
p < 0.001 for |
p < 0.001 for |
|
|
inferiority |
superiority |
non-inferiority |
non-inferiority, p = 0.01 for superiority |
|
Relative risk (95% CI) of ischaemic stroke versus warfarin |
1.10 (0.89–1.40) |
0.76 (0.60–0.98) |
0.94 (0.75–1.17) |
0.92 (0.74–1.13) |
|
Relative risk (95% CI) of haemorrhagic stroke versus warfarin |
0.31 (0.17–0.56) |
0.26 (0.14–0.49) |
0.59 (0.37–0.93) |
0.51 (0.35–0.75) |
|
Relative risk (95% CI) of intracranial bleed versus warfarin |
0.31 (0.20–0.47) |
0.40 (0.27–0.60) |
0.67 (0.47–0.93) |
0.42 (0.30–0.58) |
|
Relative risk (95% CI) of major bleeding versus warfarin |
0.80 (0.69–0.93) |
0.93 (0.81–1.07) |
1.04 (0.90–1.20) |
0.69 (0.60–0.80) |
|
Relative risk (95% CI) of gastrointestinal bleeding versus warfarin |
1.10 (0.86–1.41) |
1.50 (1.19–1.89) |
1.61 (1.30–1.99) |
0.89 (0.70–1.15) |
|
Relative risk (95% CI) myocardial infarction versus warfarin |
1.29 (0.96–1.75) |
1.27 (0.94–1.71) |
0.81 (0.63–1.06) |
0.88 (0.66–1.17) |
|
Relative risk (95% CI) of all cause death versus warfarin |
0.91 (0.80–1.03) |
0.88 (0.77–1.00) |
0.85 (0.70–1.02) |
0.89 (0.80–0.99) |
|
|
Efficacy |
Safety |
|
|
Mortality |
|
stroke and systemic |
major bleeding |
gastrointestinal |
Intracranial |
|
|
|
embolism |
|
bleeding |
hemorrhage |
|
|
|
Dabigatran 110 mg BID |
Non-inferior |
Decreased |
Comparable |
Decreased |
Comparable |
|
Dabigatran 150 mg BID Dabigatran pooled EU |
Superior Superior |
Comparable Decreased |
Increased Comparable |
Decreased Decreased |
Comparable Decreased |
|
Rivaroxaban |
Non-inferior |
Comparable |
Increased |
Decreased |
Comparable |
|
Apixaban |
Superior |
Decreased |
Comparable |
Decreased |
Decreased |
|
|
Dabigatran |
Revaroxaban |
Apixaban |
Edoxaban |
|
Renal clearance,% |
80 |
35 |
27 |
50 |
|
Dosing for nonvalvular AF |
150 mg twice daily |
20 mg daily with evening meal |
5 mg twice daily |
If CrCL>50ml/min to≤95ml/min: 60mg daily |
|
|
When CrCI 30 to 49 ml/min: |
|
2.5 mg twice daily if the patient has |
If CrCL 15 to 49 ML/min:30 mg daily |
|
Dosing consideration for nonvalvular AF with renal adjustments |
150 mg twice daily is ppssible but 110mg twice daily should be considered Note:75 mg twice daily approved in United states only: . CrCl 15 to 30ml/min |
If CrCI is 15 to 49ml/min: |
Aged ≥ 80 years .weight ≤ 60kg SCr≥ 1.5 mg/dl |
In United States obly if CrCI >95 ml/min: do not use: may have an increased risk of ischemic stroke compared with warfarin |
Choosing the precise anticoagulant for SPAF
Complications, convenience, Compliance, confidence & cost are the 5 Cs for effective anticoagulation management.[11] There are two important decisions that must be made with respect to anticoagulation in AF. First, should a patient with AF required anticoagulant treatment for thromboprophylaxis and, secondly, which anticoagulant should be used.
As per 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation, Oral Anticoagulant (OAC) is recommended for stroke prevention in AF patients with CHA2DS2-VASc score ≥ 2 in men or ≥ 3 in women (Class I and level A evidence). Antiplatelet therapy alone (monotherapy or aspirin in combination with clopidogrel) is not recommended for SPAF. SPAF patients who are eligible for OAC, NOACs are recommended in preference to VKAs (excluding patients with mechanic al heart valves or moderate-to-severe mitral stenosis) (Class I and level A evidence). If a VKA is used, a target INR of 2.0 - 3.0 is recommended, with individual TTR ≥70%. (Class I & level B evidence).[12]
Which anticoagulant class to choose: VKAs or NOACs?
In India, Vitamin K antagonists are widely used oral anticoagulants. Vitamin K antagonists (VKAs) such as warfarin & Acenocoumarol have long been the mainstay of stroke prevention in patients with atrial fibrillation (AF). Nevertheless, the use of VKAs in clinical practice is always challenging due to problems such as drug-drug and drug-food interactions, a narrow therapeutic index and unpredictable anticoagulant effects, all of which result in the need for regular laboratory monitoring only advantage is cost of therapy.[11] As per ESC 2020, If a VKA is used, a target INR of 2.0 - 3.0 is recommended, with individual TTR ≥70% which is extremely challenging in clinical practice. In a systemic review, Wan et al. found that poor control of anticoagulation associated with increased bleeding and thromboembolic risk. Indeed, it has been shown that when TTR falls below 50%, stroke outcomes are worse than if the patient remained untreated, and bleeding risk is higher.[13], [14]
Which NOAC to Choose?
Direct comparison of the results from large, international, multicentre randomized control trials of NOACs versus warfarin for SPAF is difficult due to differences in the mean CHADS2 score, TTR and rates of stroke and systemic embolism and haemorrhage in the warfarin arms of the trials.
Factors to considered while selecting appropriate NOACs
Medical conditions like renal & liver function, concomitant medications, age of patient, adherence and patient preference, patient at very high risk of ischemic stroke, patient with very high risk of bleeding & cost of therapy should be considered while selecting NOACs.
Patients With Renal Impairment
Renal impairment is related with an increased incidence of stroke (secondary to co-existent risk factors) and is an independent risk factor for haemorrhage (HR 1.27, 95% CI 1.09–1.49).[15] Both the incidence of AF and renal impairment increase with advancing age; therefore, determining suitable and safe anticoagulation for this growing population is an important clinical issue.
VKAs have a poor safety profile in patients with non-dialysis dependent severe chronic kidney disease [estimated glomerular filtration rate (eGFR) <30], with these patients at a higher risk of major bleeding events and stroke compared to individuals with moderate renal impairment (eGFR 30–60) or compared to individuals with moderate renal impairment (eGRF 30– 60 ) or those without chronic kidney disease (eGFR > 60).[16] Limited data on the safety and efficacy of NOACs in patients with AF and renal impairment are available.
Dabigatran has the greatest extent of renal elimination (80%), while 35%, and 27% of rivaroxaban, and apixaban, respectively, are cleared via the kidneys.
There are no data on the use of NOACs in AF patients after kidney transplantation. NOACs are used in such patients, the dosing regimen should be selected according to the renal function, and caution is needed concerning possible Dru Drug interaction between the NOAC and concomitant immunosuppressive therapies.[17]
Elderly Patients
The prevalence of AF is estimated to be between 10.0% and 17.8% in patients over the age of 85. The prevalence of AF rises with age.[18], [19] Meta-analysis of the trials involving dabigatran, rivaroxaban and apixaban showed that NOACs were more effective than warfarin therapy in the SPAF; individual drugs were all found to be noninferior to warfarin in the elderly. NOACs were not associated with increase in major or clinically relevant bleeding events in patients over 75 years of age.[20]
Patients with high risk of haemorrhage
The HAS-BLED score can be used to predict the risk of haemorrhage, with a score of 3 or greater signifying significant risk. Compared to warfarin, each of the NOACs reduces the incidence of intracranial haemorrhage. Patients at high risk of gastrointestinal haemorrhage, it is reasonable to avoid high-dose dabigatran and rivaroxaban. In patients with high HAS-BLED scores who have suffered major haemorrhage, low-dose dabigatran, apixaban are all suitable choices of anticoagulant, but the risk of haemorrhage should be balanced carefully against the risk of stroke and patients’ personal preferences.[4] BID dosing of NOACs like apixaban and Dabigatran causes lower peak–trough ratio of blood levels (i.e., lower peaks and higher troughs), compared with once a day dosing. Rivaroxaban had higher overall rates of GI Bleed (3.2 vs. 2.5 events per 100 person-years; hazard ratio [HR], 1.42 [95% CI, 1.04 to 1.93]) and major GI Bleed (1.9 vs. 1.4 events per 100 person-years; HR) compared with apixaban. Dabigatran was linked with lower rates of upper GI Bleed than rivaroxaban.[21]
Patients with existing coronary artery disease (CAD) or peripheral vascular disease
AF with CAD or PVD often co-exist. There is considerable scope for the overlap of anticoagulant & antiplatelet treatments in patients with CAD or peripheral vascular disease and concurrent AF. Single and dual antiplatelet therapies provide first line treatments for patients with coronary artery disease (CAD) or peripheral artery disease (PAD).[4]
In all four trials comparing NOACs to warfarin (VKA) in patients with AF, concurrent aspirin use was associated with higher incidence of major haemorrhage regardless of the treatment arm. The occurrence of major haemorrhage when a NOAC was co-administered with aspirin was consistently lower than that seen with warfarin. NOACs offer promising safety advantages compared to warfarin when used in combination with antiplatelet therapy, but this must be confirmed in future studies.[4]
Patients with a high risk of stroke or a previous TIA/stroke
A recent meta-analysis of the ROCKET-AF, RE-LY, and ARISTOTLE trials demonstrated that rivaroxaban, dabigatran, and apixaban were all noninferior to warfarin in this respect. Apixaban was associated with the lowest risk of stroke or systemic embolism in patients who had already suffered a previous stroke or TIA although this finding was not statistically significant.[22]
Availability of reversal agents
One of the important advantages of VKAs over NOACs is availability of reversal agent. Recently idarucizumab, a humanized monoclonal antibody fragment approved and available which binds and is an effective reversal agent for dabigatran.[23] NOACs are having shorter half-lives compared with VKAs, meaning the requirement for reversal is likely to be less with NOACs than with VKAs.
Conclusion
Recent development of newer-generation, direct oral anticoagulants have been clinically authenticated to help overcome shortcomings of VKA therapy. These medications largely have a more consistent pharmacokinetic profile allowing once- or twice-daily administration without routine PT /INR monitoring. Less Drug-drug interactions. Mechanisms of action of DOACs directly inhibit different portions of the coagulation cascade. Dabigatran functions by direct inhibition of thrombin. Rivaroxaban, apixaban inhibit factor Xa. Selecting and adhering to anticoagulant therapy remains challenging for physicians and patients with AF.
Source of Funding
None.
Conflict of Interest
None.
References
- Bai Y, Wang YL, Shantsila A, Lip GYH. The global burden of atrial fibrillation and stroke: a systematic review of the epidemiology of atrial fibrillation in regions outside North America and Europe. Chest. 2012;152(4):1489-98. [Google Scholar]
- Friberg L, Hammar N, Rosenqvist M. Stroke in paroxysmal atrial fibrillation: report from the Stockholm Cohort of Atrial Fibrillation. Eur Heart J. 2010;31(8):967-75. [Google Scholar]
- LJ, Adams D, Brown RJ. Stroke in paroxysmal atrial fibrillation: report from the Stockholm Cohort of Atrial Fibrillation. Circulation. 2010;31(8):46-215. [Google Scholar]
- Shields AM, Lip GYH. Choosing the right drug to fit the patient when selecting oral anticoagulation for stroke prevention in atrial fibrillation. (Review). J Intern Med. 2015;278(1):1-18. [Google Scholar]
- Gopalakrishnan S, Narayanan S. Oral Anticoagulants: Current Indian Scenario. . 2013. [Google Scholar]
- Trailokya A, Hiremath JS. Dabigatran - the First Approved DTI for SPAF. J Assoc Physicians India. 2018;66(4):85-90. [Google Scholar]
- Trailokya A, Hiremath JS. Dabigatran - the First Approved DTI for SPAF. J Assoc Physicians India. 2018;66(4):85-90. [Google Scholar]
- Morgan CL, Mcewan P, Tukiendorf A. Warfarin treatment in patients with atrial fibrillation: observing outcomes associated with varying levels of INR control. Thromb Res. 2009;124(1):37-41. [Google Scholar]
- Steffel J, Collins R, Antz M, Cornu P, LD, Haeusler KG. European Heart Rhythm Association Practical Guide on the Use of Non-Vitamin K Antagonist Oral Anticoagulants in Patients with Atrial Fibrillation. Europace. 2021;23(10):1612-76. [Google Scholar]
- Kovacs RJ, Flaker GC, Saxonhouse SJ, Doherty JU, Birtcher KK, Cuker A. State of the art review. J Am Coll Cardiol. 2015;65(13):1340-60. [Google Scholar]
- Haemost T. Efficacy and safety of edoxaban in comparison with dabigatran, rivaroxaban and apixaban for stroke prevention in atrial fibrillation. An indirect comparison analysis. Thromb Haemost. 2014;111(5):981-9. [Google Scholar]
- Trailokya A. Acenocoumarol in Thromboembolic Disorders. Cardiovasc Pharm Open Access. 2015;4(4). [Google Scholar]
- Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Lundqvist CB. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association of Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2020;42(5):373-498. [Google Scholar]
- Wan Y, Heneghan C, Perera R. Anticoagulation control and prediction of adverse events in patients with atrial fibrillation: a systematic review. Circ Cardiovasc Qual Outcomes. 2008;1(2):84-91. [Google Scholar]
- Giannakoulas G, Farmakis D, Davlouros P, Giamouzis G. Direct Oral Anticoagulants in Nonvalvular Atrial Fibrillation: Practical Considerations on the Choice of Agent and Dosing. Cardiology. 2018;140(2):126-32. [Google Scholar]
- Friberg L, Benson L, Lip GY. Balancing stroke and bleeding risks in patients with atrial fibrillation and renal failure: the Swedish Atrial Fibrillation Cohort study. Eur Heart J. 2015;36(5):297-306. [Google Scholar]
- Kooiman J, Rein NV, Spaans B. Efficacy and safety of vitamin K-antagonists (VKA) for atrial fibrillation in non- dialysis dependent chronic kidney disease. PLoS One. 2014;9(5). [Google Scholar]
- Heidbuchel H, Verhamme P, Alings M, Antz M, Diener HC, Hacke W. Updated European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist anticoagulants in patients with non-valvular atrial fibrillation. Europace. 2015;17(10):1467-1507. [Google Scholar]
- Heeringa J, Kuip DAVD, Hofman A. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur Heart J. 2006;27(8):949-53. [Google Scholar]
- Langenberg M, Hellemons BS, Ree JWV. Atrial fibrillation in elderly patients: prevalence and comorbidity in general practice. BMJ. 1996;313(7071). [Google Scholar]
- Sardar P, Chatterjee S, Chaudhari S. New oral anticoagulants in elderly adults: evidence from a meta-analysis of randomized trials. J Am Geriatr Soc. 2014;62(5):857-64. [Google Scholar]
- Ingason AB, Jóhann P, Arnar S. Rivaroxaban Is Associated With Higher Rates of Gastrointestinal Bleeding Than Other Direct Oral Anticoagulants : A Nationwide Propensity Score-Weighted Study. Ann Intern Med. 2021;174(11):1493-1502. [Google Scholar]
- Schiele F, Ryn JV, Canada K. A specific antidote for dabigatran: functional and structural characterization. Blood. 2013;121(18):3554-62. [Google Scholar]
- Abstract
- Introduction
- Which NOAC to Choose?
- Patients With Renal Impairment
- Elderly Patients
- Patients with high risk of haemorrhage
- Patients with existing coronary artery disease (CAD) or peripheral vascular disease
- Patients with a high risk of stroke or a previous TIA/stroke
- Availability of reversal agents
- Conclusion
- Source of Funding
- Conflict of Interest
- References
How to Cite This Article
Vancouver
Trailokya AA, Roy DG, Kerkar P, Merchant S, Sethi R, Karnik R, Manchanda SC, Shetty S, Jadhav U, Vijan V. Right selection of oral anticoagulation for stroke prevention in atrial fibrillation [Internet]. Indian J Pharm Pharmacol. 2022 [cited 2025 Oct 07];9(3):164-170. Available from: https://doi.org/10.18231/j.ijpp.2022.029
APA
Trailokya, A. A., Roy, D. G., Kerkar, P., Merchant, S., Sethi, R., Karnik, R., Manchanda, S. C., Shetty, S., Jadhav, U., Vijan, V. (2022). Right selection of oral anticoagulation for stroke prevention in atrial fibrillation. Indian J Pharm Pharmacol, 9(3), 164-170. https://doi.org/10.18231/j.ijpp.2022.029
MLA
Trailokya, Abhijit Anil, Roy, Debanu Ghosh, Kerkar, Prafulla, Merchant, Shahid, Sethi, Rajeev, Karnik, Rajiv, Manchanda, S. C., Shetty, Sadanand, Jadhav, Uday, Vijan, Vinod. "Right selection of oral anticoagulation for stroke prevention in atrial fibrillation." Indian J Pharm Pharmacol, vol. 9, no. 3, 2022, pp. 164-170. https://doi.org/10.18231/j.ijpp.2022.029
Chicago
Trailokya, A. A., Roy, D. G., Kerkar, P., Merchant, S., Sethi, R., Karnik, R., Manchanda, S. C., Shetty, S., Jadhav, U., Vijan, V.. "Right selection of oral anticoagulation for stroke prevention in atrial fibrillation." Indian J Pharm Pharmacol 9, no. 3 (2022): 164-170. https://doi.org/10.18231/j.ijpp.2022.029
