- Visibility 22 Views
- Downloads 6 Downloads
- DOI 10.18231/j.ijpp.2021.028
-
CrossMark
- Citation
Spectrum of Botulin toxin
- Author Details:
-
Sunil Chaudhry *
Introduction
Botulism is most commonly caused by neurotoxins produced by C. botulinum but C. baratii produces similar neurotoxins. Botulinum toxin is the most potent toxic substance in nature. The neurotoxins which cause botulism are the most potent toxins currently known and cause paralysis through the inhibition of acetylcholine release in human nerve endings.
Clostridium botulinum toxins are grouped as
Group I - can produce toxins specifically A, B, or F which are proteolytic.
Group II - can produce toxins specifically B, E, or F, which are non proteolytic.
Group III - can produce toxins C or D.
Group IV - can produce toxin G (does not cause neuroparalytic illness). Botulin Toxin A: duration of paralysis is related to toxin dose; the paralysis time doubled with every 25% increase of the toxin concentration.For type B, the duration of paralysis was increased with more dose. Type E toxin had the shortest duration of action.
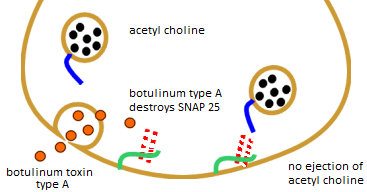
Mode of action of Botulin toxin
The mechanism of action of Botulin neurotoxins (BoNT) on the nerve terminals is as follows:
SNAP-25 is a component of the SNARE protein complex, which is involved in the exocytotic release of neurotransmitters during synaptic transmission.
SNAP-25 cleaved by BoNT display different inhibition effects on membrane fusion.
BoNT‐A causes muscular weakness and paralysis by preventing acetylcholine (ACh) release into the synaptic cleft at nerve endings within striated muscle, smooth muscle, and autonomic exocrine glands.
Botulin toxin A and B
Botulinum toxin type B had a slightly faster onset of action than type A. All patients responded to type B quickly, whereas some had a delayed response to type A.
|
Features |
Type A |
Type B |
|
Other names |
Onabotulinumtoxin ONA, |
Rimabotulinumtoxin B |
|
Abobotulinumtoxin A, |
||
|
Incobotulinumtoxin A |
||
|
Molecular weight |
150-900 kD |
700 kD |
|
Brands |
Botox, Dysport, Xeomin |
Myobloc |
|
Indications |
Moderate to severe glabellar lines, crow’s feet, blepharospasm, cervical dystonia (Cosmetology) |
Cervical dystonia and other indications |
|
Dilution |
0.9% saline without preservatives |
Ready to use. No reconstitution required. |
|
Composition |
Botulinum toxin type A, human serum albumin, and NaCl. Additional lactose and trace cow’s milk protein for Dysport; sucrose for Xeomin |
Botulinum toxin type B, human serum albumin, NaCl, and sodium succinate |
|
Preparation |
50, 100, 200, 300, 500 units/vial |
2,500, 5,000, or 10,000 units/vial |
|
Mode of action |
Cleaves with SNAP 25 (SNAREs are small, abundant, sometimes tail-anchored proteins) |
Cleaves with VAMP (vesicle-associated membrane protein) |
|
Duration |
Up to 16 weeks |
12 to 16 weeks |
|
Side Effects |
-Localized pain, swelling or bruising |
-Localized pain or muscle weakness |
|
-Headache |
-Dry mouth or nausea |
|
|
-Dryness of the eyes |
-Upset stomach |
|
|
-Drooping eyelids and brows |
-Headache or joint and back pain |
|
|
-Crooked smile |
-Drowsiness |
|
|
|
-Drooping eyelids |
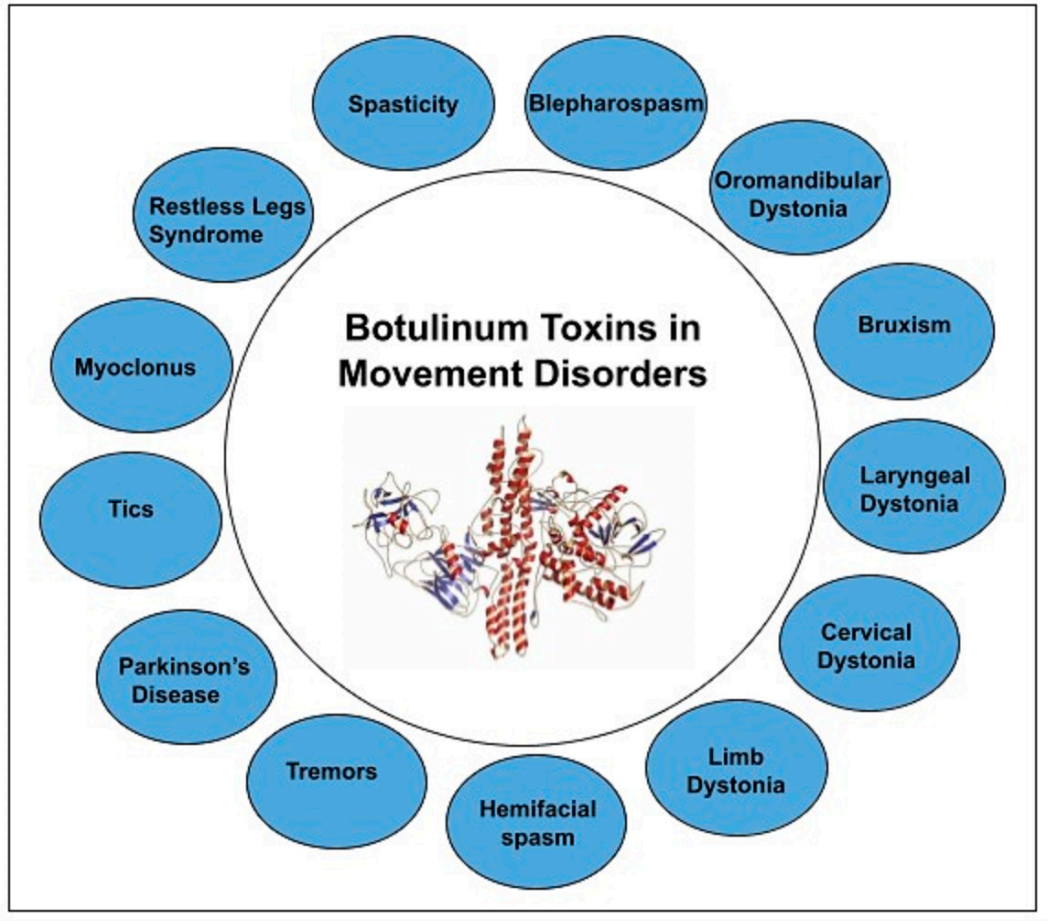
Indications for Botulin toxin therapy
|
Focal Dystonias |
Bruxism |
|
Blepharospasm |
Nystagmus |
|
Cervical Dystonias |
Tension Headaches |
|
Laryngeal Dystonias |
Back spasm |
|
Occupational cramps |
Vaginismus |
|
Focal Dystonias |
Strabismus |
|
Involuntary movements |
Spasticity |
|
Hemifacial spasm |
Lower urinary tract spasm |
|
Tics |
Detrusor sphincter dyssynergia and overactivity incontinence |
|
Voice, head and limb tremors |
Urinary retention after suburethral sling |
|
Palatal myoclonus |
|
|
Axillary hyperhidrosis |
|
|
Cosmetic – Glabellar facial liners |
|
Neurological and ophthalmological indications of Botulin toxin
There is a correlation between the amount of BT applied and the duration of its action. The therapeutic effect of Botulin toxin is temporary and usually lasts between three to ten months, depending on the approved indication and on the individual patient.
Dystonia
BT can be used to treat focal dystonias including cranial, pharyngolaryngeal, cervical and limb dystonias. In segmental and generalized dystonias. Botox doses of up to 840 MU have been used with safety.[3]
Periocular, mandibular and perioral muscles are affected in Cranial dystonias. BT (Botulin Toxin) therapy can be used in all of these muscles successfully, either when they occur in isolation or when they occur in various combinations. BTX (Botulin Toxin) is safe and highly effective in long-term treatment of patients with cervical dystonias, with only mild and well- tolerated side-effects.
Pharyngolaryngeal dystonia Tonic or clonic dystonia of the pharynx can produce dysphagia and dyspnoea BT injections into the posterior pharynx can easily be placed transorally and are effective. Doses range between 20-40 MU of ONA are used.[4]
Focal dystonia is a common, invalidating neurologic condition characterized by involuntary, sustained muscle contractions causing twisting movements and abnormal postures in one body part. Local injections with Botulinum toxin A (BTX A) are safe and effective in the treatment of focal dystonia.
In cervical dystonia and blepharospasm, BTX A injections have become the treatment of choice.
Leg and foot dystonia
Hip adduction, ankle plantar flexion and equinovarus postures respond well to BT therapy. Pain and functional outcomes are improved. 6-Minute Walk Test (6MWT), gait velocity also improved.
Botulinum toxin therapy has been reported successful in strabismus surgery for patients with binocular vision. Botulinum toxin causes paralysis of injected extraocular muscle within 2-4 days after injection and lasts clinically for at least 5-8 week.[5]
Idiopathic hemifacial spasm
Consists of irregular, unilateral clonic twitching or more sustained contractions of the facial muscles. insidious in onset in 5th or 6th decades, affecting females more than males, it often starts in the orbicularis oculi and progresses in a stereotyped way, to involve all the facial muscles, including the platysma. Botulinum toxin A (15, ug) was injected in 1 ml saline in four divided doses into the orbicularis oculi, with significant reduction in contractions.[6]
Onabotulinum toxin ONA was found to be an effective treatment for ocular tics, providing both subjective and objective benefit for a subset of patients.[7]
Nystagmus Botulinum toxin has been injected into the medial rectus and lateral rectus muscles for the treatment of acquired pendular nystagmus. Retrobulbar injection often induces diplopia and ptosis. After injection of 25 units of botulinum A toxin, visual acuity improved significantly.[8]
Bruxism is a repetitive activity of the masticatory muscles characterized by tightening or grinding of teeth. It is a common condition with an adult prevalence ranging between 8 and 31%. Botulinum toxin injections are equally as effective as nocturnal oral splint for bruxism. 25 U of onabotulinum toxin A in each masseter, but may increase the dosage up to 300 U to include the masseters and temporalis muscles for optimal benefit.
Botulinum toxin injections are used to treat motor and phonic tics in patients with Tourette’s syndrome. BTX-A appears a safe and effective treatment for simple motor tics and retains its efficacy after long-term treatment.[9]
Frontal tension headaches the incidence of tension headache is 78% and 24–37% patients had several times in a month,. Botulinum toxin type A was well tolerated, with no significant adverse events. Injection with 12.5 IU of botulinum toxin A into the corrugator supercilii muscle on both sides (a total of 25 IU). Following injection, patients had less pain for approximately two months.[10]
The technique of treatment for Chronic Low Back pain included covering the whole length of the lumbar erector spinae with one injection given at each lumbar level regardless of pain, tenderness, or trigger point location(s). The dose per injection site was 50 U (Botox), with the total dose per session not to exceed 500 U.[11]
Migraine
The Cochrane review concluded that people with chronic (persisting) migraine treated with botulinum toxin injections had two fewer migraine days per month than people treated with placebo. Small amount of botulinum toxin are injected into the muscles of the head and neck. Injections are usually given every 12 weeks with maximal effect peak achieved by about 2-3 weeks. For chronic migraine, the recommended dilution is 200 Units/ 4ml or 100 units / 2ml, with final concentration of 5 units /0.1ml.[12]
The efficacy of botulinum toxin in various pain syndromes is a result of mechanisms other than a reduction in muscle tone.
Inhibition of release of substances that sensitise muscle nociceptors;
An effect on spindle afferents favourably altering the firing pattern of supraspinal projections and changing the central sensory processing;
Suppression of neurogenic inflammation;
Inhibition of substance P, glutamate, and other peptides and neurotransmitters involved in mediating pain.[13]
Spasticity
Spasticity is a common disabling disorder in adult subjects suffering from stroke, brain injury, multiple sclerosis (MS) and spinal cord injury (SCI).
Benefits of Botox in Spasticity:
Significantly improved gait pattern.
Improvement in positioning and range of motion.
Decreased pain in stiff muscles.
Reduction of spasticity and greater ease in stretching.
Dosing for Toxin A or Botox is based on different clinical trials.
For upper limb spasticity, flexible dosing up to 400 Units was studied.
For lower limb spasticity, a dose of 300 Units to 400 Units divided among 5 muscles was studied.
Early open label studies investigated the use of BTX-A in people with upper limb spasticity secondary to stroke and all supported its use and provided evidence of its effectiveness in reducing muscle tone. Treatment with the highest dose resulted in a statistically significant mean decrease in muscle tone for up to 6 weeks after injection.
Advantages of Botulin A therapy in spasticity
Delay deformities and contractures
Delay surgery in cerebral palsy
Facilitate physiotherapy, occupational therapy and orthosis use
Pain relief[14]
Low back pain
Botox into neck muscles significantly reduced neck pain and chronic back pain. Botulinum toxin A was prepared by combining vacuum-dried BoNT-A with preservative-free 0.9% saline to a concentration of 100 units/ml. Injections were made using a 1 cc -tuberculin syringe, unilaterally or bilaterally based on the predominant pattern of pain distribution.
Mode of spasm relief
Reduction of muscle spasm due to blocking acetylcholine release from pre-synaptic vesicles, and decrease (substance P and bradykinin) from the dorsal root ganglia.
Decreased discharge of sympathetic neurons, thereby relieving chronic pain.
Head tremor Intractable head tremor, which does not respond to oral medications respond to treatment with BTX injections. BTX treatment is usually effective in reducing the tremor amplitude and improving function 17].
Other specified conditions
Blepharospasm generally begins as excessive blinking, usually accompanied by feelings of dryness or irritation of the eyes. The estimated prevalence is 5 per 100,000 people. The initial recommended dose is 1.25 Units to 2.5 Units (0.05 mL to 0.1 mL volume at each site). The recommended dilution to achieve 1.25 Units is 100 Units/8 mL; for 2.5 Units it is 100 Units/4 mL Adverse effects for periocular injections are relatively common, but usually mild.
Induce ptosis/Reduce lid retraction
Botulin toxin can be used to chemically denervate the eyelids to induce ptosis. Botulinum toxin A-induced ptosis is a good alternative to surgical tarsorrhaphy in thyroid eye disease (TED), neurotrophic keratopathy or Bell’s palsy.
Botulinum toxin is a highly effective temporary treatment for involutional entropion with few complications and no adverse effects. Injection of 5 to 10 units of Botulin toxin A into the pretarsal or preseptal orbicularis muscle can eliminate the spastic component of the entropion.[15]
Meige syndrome is a rare neurological movement disorder characterized by involuntary and often forceful contractions of the muscles of the jaw and tongue. Symptoms typically begin in middle-age between 40-70 years. The peak effect of BTX was noticed within 7 days. The average duration of relief in symptoms was 11.5 weeks in our study, which was similar to the previously reported series (range: 9–16 weeks).[16]
Vaginismus is characterized by recurrent or persistent involuntary contraction of the perineal muscles surrounding the outer third of the vagina. Lower doses of Botox were used to preserve some of the muscular activity of the vagina. Higher doses (100 to 150 units of Botox) were found to be more effective in achieving complete temporary relaxation of the vagina.
Treatment with Botulinum toxin was effective in 89% of patients with chronic uncomplicated anal fissure. Botulinum toxin (e.g, onabotulinum toxin A [BOTOX®]) has been used to treat acute and chronic anal fissures. It is injected directly into the internal anal sphincter, in effect performing a chemical sphincterotomy. The effect lasts about 3 months, until nerve endings regenerate.
Diseases of Urinary Tract
Botulinum toxin in overactive bladder and neurogenic bladder.is effective measure. BoNT-A blocked neurotransmitter release after injection into the detrusor muscle and reduced muscarinic receptor M2 activation in the nerve terminal which do not respond to anticholinergic therapy. Therapy for urinary incontinence consists of 30 intradetrusor injections (Botox® (range 100-400 U)) via cystoscopy.
Local injections of Botulinum toxin type A (BTX-A) are an effective and safe solution for primary bilateral axillary hyperhidrosis. If the traditional treatments are often ineffective and difficult to tolerate. Intradermal injection of botulinum toxin A is an effective and safe therapy for severe axillary hyperhidrosis. The injection of botulinum toxin for the treatment of axillary hyperhidrosis is a simple procedure that is relatively quick to perform and has a low risk of complications.[17]
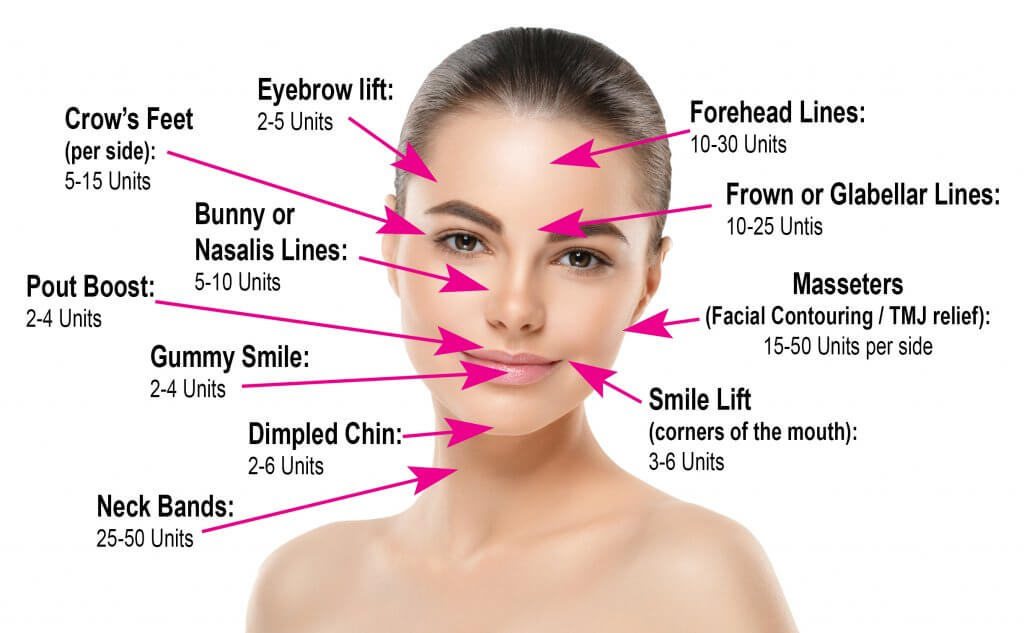
Botulin in Cosmetology
Patients with dynamic wrinkles demonstrate the most dramatic improvements from botulinum toxin injection and are ideal candidates for treatment Patients with static wrinkles that are visible at rest can also be treated but results are slower and patients may require two or three consecutive botulinum toxin treatments for significant improvements. Wrinkles are formed by dermal atrophy and repetitive contraction of underlying facial musculature. Injection of small quantities of botulinum toxin into specific overactive muscles causes localized muscle relaxation that smooths the overlying skin and reduces wrinkles. Dermatologists use botulinum toxin therapy to diminish signs of aging and to treat a medical condition called hyperhidrosis (excessive sweating). It may take two to three, and in rare cases up to five days, after treatment. Botulin toxin can be very effective in reducing wrinkles due to muscle contractions, it has no effect in reducing the fine lines on the face caused by sun damage, and lines due to sagging of facial skin.
|
Frown Lines |
Crows Feet |
|
Horizontal Forehead Lines |
Vertical Lip Lines |
|
Bunny Lines |
Gummy Smile |
|
Downturned corners of mouth |
Chin Dimpling |
|
Jawline Definition |
Masseter Hypertrophy |
|
Platysmal bands |
Facial Asymmetry |
|
Injection reactions |
Undesired botulinum toxin effects |
|
Anxiety or vasovagal episode |
Allergic reaction |
|
Ecchymosis |
Antibodies against botulinum toxin |
|
Erythema, edema, and tenderness |
Blepharoptosis |
|
Paresthesia or dysesthesia |
Distant spread from the injection site |
|
Headache, Infection |
Facial asymmetry |
Use of botulinum toxins in cancer pain symptomatically
Local injection of BoNT improved neuropathic pain and local muscle spasm at/or close to the site of surgery and radiation. Botulinum toxin significantly improved pain scores and masticator spasms (oromandibular dystonia).[19]
Conclusion
The novel mode of action of Botulin toxin is neuromuscular block by inhibiting the released of acetylcholine resulting in partial, local, flaccid muscle paralysis, which helps to reduce some of the abnormal muscle contractions. The therapeutic effect of toxin injection usually is apparent in 7-10 days. Optimal response from the toxin is reached in approximately 4-6 weeks and lasts for an average of 12 weeks. Injections usually are repeated every 3-4 months. Rare feature with botulinum toxin injections is formation of antibodies in less than 1%, which can render treatments ineffective. Botulin toxin is effective tool in hands of expert neurologist, urologist or dermatologist who can titrate the dose depending on the clinical condition of the patient.
Source of Funding
None.
Conflict of Interest
The authors declare that there is no conflict of interest.
References
- M Pirazzini, O Rossetto, R Eleopra, C Montecucco. Botulinum Neurotoxins: Biology, Pharmacology, and Toxicology. Pharmacol Rev 2017. [Google Scholar] [Crossref]
- ST Mahajan, L Brubaker. Botulinum toxin: From life-threatening disease to novel medical therapy. Am J Obstet Gynecol 2007. [Google Scholar] [Crossref]
- D Dressler. Botulinum toxin for treatment of dystonia. Eur J Neurol 2010. [Google Scholar] [Crossref]
- D Dressler, FA Saberi, RL Rosales. Botulinum toxin therapy of dystonia. J Neural Transm (Vienna) 2021. [Google Scholar]
- S Wutthiphan. Botulinum toxin A in surgically overcorrected and undercorrected strabismus. J Med Assoc Thai 2008. [Google Scholar]
- JS Elston. Botulinum toxin treatment of hemifacial spasm.. J Neurol Neurosurg Psychiatry 1986. [Google Scholar] [Crossref]
- G Yahalom, A Faust-Socher, H Strauss, SF Lerman, S Hassin-Baer, OS Cohen. Botulinum Toxin for Ocular Tics. Open Neurosurg J 2015. [Google Scholar] [Crossref]
- RJ Leigh, RL Tomsak, MP Grant, BF Remler, SS Yaniglos, L Lystad. Effectiveness of botulinum toxin administered to abolish acquired nystagmus. Ann Neurol 1992. [Google Scholar] [Crossref]
- H Long, Z Liao, Y Wang. Lina Liao and Wenli LaiEfficacy of botulinum toxins on bruxism: an evidence-based review. Int Dent J 2012. [Google Scholar]
- DW Dodick, A Mauskop, AH Elkind, R DeGryse, MF Brin, SD Silberstein, . Botulinum Toxin Type A for the Prophylaxis of Chronic Daily Headache: Subgroup Analysis of Patients Not Receiving Other Prophylactic Medications: A Randomized Double‐Blind, Placebo‐Controlled Study. Headache 2005. [Google Scholar] [Crossref]
- B Jabbari. Treatment of chronic low back pain with botulinum neurotoxins. Curr Pain Headache Rep 2007. [Google Scholar] [Crossref]
- S Silberstein, N Mathew, J Saper, S Jenkins, . Botulinum Toxin Type A as a Migraine Preventive Treatment. Headache 2000. [Google Scholar] [Crossref]
- J Jankovic. Botulinum toxin in clinical practice. J Neurol Neurosurg Psychiatry 2004. [Google Scholar] [Crossref]
- Al Picelli. Adjuvant treatments associated with botulinum toxin injection for managing spasticity: An overview of the literature. Ann Phys Rehabil Med 2019. [Google Scholar]
- N Shorr, SR Seiff, J Kopelman. The Use of Botulinum Toxin in Blepharospasm. Am J Ophthalmol 1985. [Google Scholar] [Crossref]
- S Pandey, S Sharma. Botulinum toxin in Meige's syndrome: A video-based case series. Neurol India 2018. [Google Scholar] [Crossref]
- S Scamoni, L Valdatta, C Frigo, F Maggiulli, M Cherubino. Treatment of Primary Axillary Hyperhidrosis with Botulinum Toxin Type A: Our Experience in 50 Patients from 2007 to 2010. ISRN Dermatol 2012. [Google Scholar] [Crossref]
- S Nanda, S Bansal. Upper face rejuvenation using botulinum toxin and hyaluronic acid fillers. Indian J Dermatol Venereol Leprol 2013. [Google Scholar] [Crossref]
- R Ansiaux, B Gallez. Use of botulinum toxins in cancer therapy. Exp Opin Investig Drugs 2007. [Google Scholar] [Crossref]
- Introduction
- Mode of action of Botulin toxin
- Botulin toxin A and B
- Indications for Botulin toxin therapy
- Neurological and ophthalmological indications of Botulin toxin
- Dystonia
- Leg and foot dystonia
- Idiopathic hemifacial spasm
- Migraine
- Spasticity
- Advantages of Botulin A therapy in spasticity
- Low back pain
- Mode of spasm relief
- Other specified conditions
- Induce ptosis/Reduce lid retraction
- Diseases of Urinary Tract
- Botulin in Cosmetology
- Conclusion
- Source of Funding
- Conflict of Interest
