Introduction
Diabetic foot ulcers
DFU is one of the most significant and devastating complications of diabetes, and is defined as a foot affected by ulceration that is associated with neuropathy and/or peripheral arterial disease of the lower limb in a patient with diabetes,1 forming as a result of skin tissue in break down and exposing the layers underneath. They are most common under big toes and the balls of feet, and they can affect your feet down to the bones.2 Clinical features are Erythema, oedema, heat, and pain are signs of inflammation. Serous exudate, delayed healing, friable granulation tissue, discoloured granulation tissue, foul odour, pocketing of the wound base, and wound breakdown are thought of as signs specific to secondary wounds those healing by secondary, rather than primary intention.
Aetiology
The majority of foot ulcers appear to result from minor trauma in the presence of sensory neuropathy. Calluses, oedema, and peripheral vascular disease have been identified as etiological factors in the development of diabetic foot ulcers. There are several components that cause the emergence of diabetic foot ulcers in diabetic patients, can be divided into two major factors: Causative factor: Role of loss of sensation in foot mainly due to peripheral neuropathy (sensory, motor, autonomic), High foot plantar pressure, Micro fractures Contributive factor: Atherosclerosis, Diabetes.3
Prevalence of diabetic foot ulcer among diabetic patients
The prevalence of diabetic foot ulceration in the diabetic population is 4-10%; the condition is more frequent in older patients. It is estimated that about 5% of all patients with diabetes present with a history of foot ulceration, while the lifetime risk of diabetic patients developing this complication is 15%. The majority (60-80%) of foot ulcers will heal, while 10-15% of them will remain active, and 5-24% of them will finally lead to limb amputation within a period of 6-18 months after the first evaluation. Neuropathic wounds are more likely to heal over a period of 20 weeks, while neuro ischemic ulcers take longer and will more often lead to limb amputation.1
Treatment
Successful treatment of diabetic foot ulcers consists of debridement, offloading, amputation and infection control. Debridement consists of removal of all necrotic tissue, peri-wound callus, and foreign bodies down to viable tissue, to improve the healing potential of the remaining healthy tissue.4 Amputation is the removal of a nonviable limb and should be considered in patients with uncontrolled infections or non healing wounds.5 Infection control: Antibiotics selected to treat severe or limb-threatening infections should include coverage of gram-positive and gram-negative organisms and provide both aerobic and anaerobic coverage.6 Antibiotic therapy: cephalosporins, penicillin/beta-lactamase inhibitor congeners and Miscellaneous agents.
Materials and Methods
This was a prospective observational study of diabetic and DFU patients between September 2019 to march 2020 conducted in all departments of GSL general hospital and medical college. Sample size was 150 patients. Diabetic patients from all departments were included in the study. Diabetic patients of age 20 to 80 years were included. Patients of both genders were included. Non diabetic patients were excluded from this study. Incomplete case files were excluded. Data was collected directly from the prescriptions and case sheets of individual patients from the hospital on a specially designed data collection form, questionnaire and after filling the informed consent form from each patient.
Results
The data obtained from sample size of 150 diabetic patients in which 24 DFU cases were reported. From their patient data collection forms, the following results were obtained.
Age wise distribution
In this present study we categorized 150 diabetic patients into 6 groups based on age. More cases (50 among 150) of diabetes were seen in age group of 50-59 and more DFU cases (10 among 24) were seen in age group of 40-49. More prevalence of DFU among diabetic patients was seen in the age group of 40-49(35.7%).
Gender wise distribution
Considering the gender, when we compare between male and female diabetic patients, more cases are noted in males (76) when compared to females (74), whereas DFU cases among diabetic patients was noted in females (12) and males (12).
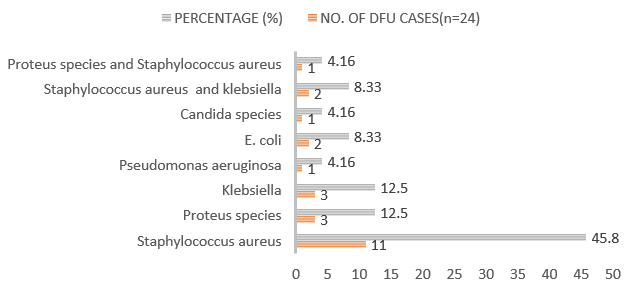
Causative organism
In the present study the most common organism cultures was staphylococcus aureus followed by proteus species, klebsiella species and the other species are pseudomonas aeruginosa, E. coli. In 1-2 cases the culture report revealed that there are multiple causative organisms.
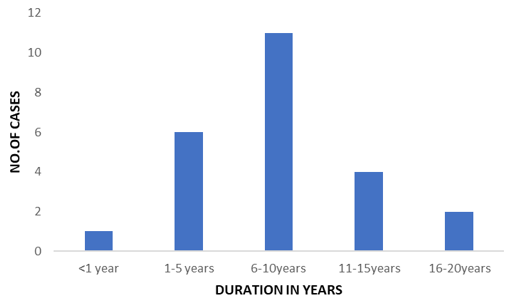
Duration of diabetes
In this study more cases of DFU were noticed in the diabetic patients with duration of 6-10 years of diabetes i.e. about 11 cases among 24.
If DFU cases doesn’t respond to antibiotic therapy, then the treatment modified to surgery. Based on surgery done in this study, the cases were divided into debridement (9) and amputation (14) and both.1
Site of lesion
In most of the DFU cases, the site of lesion was dorsum of foot followed by plantar of right foot and then by right great toe, sole of right foot and dorsum of left foot.
Prevalence of DFU among diabetic patients
This study revealed that prevalence of DFU among diabetic patients who attended to all departments of GSL General Hospital was 16% (24 DFU cases among 150 diabetic patients).
Drugs
In this study we observed that the drug therapy given to the patients with DFU includes:
Antibiotics, Anti-diabetics and Other drugs. As the main cause of this DFU is infection, the primary treatment is antimicrobial therapy. The most prescribed class of antibiotics is cephalosporins followed by nitroimidazoles, penicillins, oxazolidinones, lincosamides and others are fluoroquinolones, macrolides and combinations.
Table 4
Antibiotics
Table 5
Anti diabetics
Discussion
The study was aimed to determine the prevalence of DFU among diabetes patients and its management in all departments of GSL hospital, Rajahmundry. This study is done by using the case sheets of all the diabetic patients from all departments with sample size of 150. This study revealed that 16% (24) of all diabetic patients from all departments are prevalent to DFU and 84% (134) were not affected by DFU. Management of DFU mainly included antimicrobial therapy along with antidiabetics and other drugs included are analgesics and antacids. Diabetes mellitus, according to WHO is defined as a heterogeneous metabolic disorder characterised by common feature of chronic hyperglycaemia with disturbance of carbohydrate, fat and protein metabolism. The global prevalence of diabetic foot ulcer is about 15% of people with diabetes and precedes 84% of all diabetes related lower leg amputations. In total, we studied 150 diabetic cases at GSL Hospital, Rajahmundry in which 24 DFU cases were reported. The analysis of the study is as follows. More cases (50 among 150) of diabetes were seen in age group of 50-59 and more DFU cases (10 among 24) were seen in age group of 40-49. More prevalence of DFU among diabetic patients was seen in the age group of 40-49(35.7%). Even though 9 cases were seen in the age group of 20-29, no DFU cases were seen among those 9 patients. Similarly, 8 cases were seen in the age group of 30-39, no DFU cases were recorded among those 8 patients and the percentage of DFU among diabetes patients was 14%,18.1%,4.5% in the age groups of 50-59,60-69, ≥70 respectively. These details are given in the below table1 and figure1&2. When we considered the gender, we compared between male and female diabetic patients, more cases are noted in males (76) when compared to females (74), whereas DFU cases among diabetic patients was noted in females (12) and males(12). Percentage of DFU among male diabetes patients was 15.7%.and 16.2% among female diabetic patients. When coming to the causative organisms, most common organism cultures was staphylococcus aureus(11 i.e,45.8%) followed by proteus species (3 i.e,12.5%), klebsiella species(3i.e,12.5%) and the other species are pseudomonas aeruginosa(1i.e,4.16%), E. coli.(2 i.e,8.33%).candida species(1i.e,4.16%). In 1-2 cases the culture report revealed that there are multiple causative organisms. Duration of diabetes is also a considerable factor, this study revealed that more cases of DFU were noticed in the diabetic patients with duration of 6-10 years of diabetes i.e. about 11 cases among 24 and 1,6,4,2 DFU cases among diabetes cases with the duration of <1 year,1-5years,11-15years,16-20years respectively. If DFU cases doesn’t respond to antibiotic therapy, then the treatment modified to surgery. Based on surgery done in this study, the cases were divided into debridement (9) and amputation (14) and both (1). If DFU cases doesn’t respond to antibiotic therapy, then the treatment modified to surgery. Based on surgery done in this study, the cases were divided into debridement (9) and amputation (14) and both (1). In this study we observed that the drug therapy given to the patients with DFU includes: Antibiotics, Anti-diabetics, Other drugs. As the main cause of this DFU is infection, the primary treatment is antimicrobial therapy. The most prescribed class of antibiotics is cephalosporins followed by nitroimidazoles, penicillin’s, oxazolidinones, lincosamides and others are fluoroquinolones, macrolides and combinations.
Conclusion
The prevalence of DFU among diabetic patients is mainly due to increased blood sugar levels, infections, improper foot care, improper diet and medication adherence, injury to the foot which shows impact on foot ulcer. Our study revealed the addressed information regarding the prevalence of DFU among diabetic patients is due to lack of knowledge and uncontrolled diabetes may develop poor circulation which may further leads to wound that may heal slowly shows impact on diabetes which in turn leads to DFU. The correct therapy given to DFU patients is blood glucose control, wound debridement, advanced therapy, surgery and proper education. These approaches are used to reduce extreme morbidities and serious complications resulting from foot ulcers. The preventive measures in reduction of DFU are by educating the patients to reduce weight, good diabetic control, foot self-care practice, simple hygienic practices, regular foot examination, provision of appropriate foot wear, patient education, treatment of minor injuries can decrease the ulcer occurrence and eliminate the need for major amputation.
Acknowledgment
The authors would like to thank Dr. Ch. Sreenivasa Rao, Department of Surgery and all the staff in GSL medical college & general hospital, Rajanagaram for their clinical support. Finally we would like to thank everybody who was important to the successful realization of thesis, as well as expressing.