Introduction
National Mental Health Survey concludes nearly 10% of the population are suffering from Common Mental Disorders (CMDs), including substance use, anxiety disorder, and depression. Nearly 1 in 20 are suffering from depression out of which 1% of the population turned out to be at high risk for suicide with the age group of 40 to 49.1
Prescription is a written medicolegal document given by a registered medical practitioner to the patient which helps in the reflection of quality health care service. A correct pattern of prescription is one of the initial steps to promoting the rational use of medicine.
Irrational prescription is a challenging and extremely serious global problem leading to harmfulness. Irrational prescription can lead to drug-related problems (DRP) which include adverse drug reaction (ADR), unwanted treatment, polypharmacy, and financial problems with an incidence rate of 25%.2 Such sort of DRPs is common in hospitalized patients and can result in mortality and morbidity.3 National list of essential medicine helps to overcome DRP and improves patient compliance.4
Drug-Drug interactions (DDI) exhibit their influence on drug effects and also play an important role in either reducing the efficacy and therapeutic effect of the drug or it can lead to drug toxicity.5 Such potential risk of drug-drug interaction can be reduced by the health care professional only if the prescriber has an optimal idea about the drug along with a clear view on how to combine rational prescribing.6
According to WHO, 50% of treatment regimens are inadequate in terms of instructing, labeling, or dispensing the medicine to the patient.7 This leads to a potential reflection on overall health care expenditure, where 25 to 70% accounts for medical expenses.8 Such a lag in conveying the medical instructions through prescription can be drastically reduced by conducting regular prescription auditing and also by giving periodic awareness, updates, and importance about the prescription to the prescribers. World Health Organization (WHO) core prescribing is one of the key indicators which can be followed by health care professionals to streamline the prescription patterns which eventually helps in a better outcome for the health care system.9
Though prescription studies are available, many of them focus on the prevalence of psychiatric disorders and the pattern of prescribing antidepressants. This study aims to assess the prescription pattern of a tertiary care hospital in South India using the WHO-recommended core prescribing indicators.
Materials and Methods
A prospective cross-sectional study was conducted in the Psychiatry outpatient department (OPD) of a tertiary care hospital after obtaining prior permission and clearance from the Institutional Ethics Committee. Patients of both gender coming to the pharmacy during the OPD hours from 10 AM to 1 PM with the Psychiatry prescription were included as study participants and the data was collected for a period of 2 months (April and May 2022). Patients reaching the pharmacy with a prescription from other departments and patients with follow-up prescriptions were excluded from the study. To assess the drug use pattern in health facilities WHO recommends at least 600 prescriptions, hence 600 prescriptions were collected.9 Confidentiality of the patient was maintained throughout the study and the study was conducted as per the Good Clinical Practice (GCP) guidelines.
The complete analysis of the prescriptions was achieved with the help of the presence or absence of general parameters namely: demographic details of the patient (Hospital ID, patient name, address, age/DOB, and gender) and prescriber’s information (Consultant name, registration number of consultant, date, and signature)
Legibility of prescription was recorded by a subjective grading scale based on two independent investigators:
The collected data were also assessed for other factors in the prescription such as Drug-drug interaction (DDI) and for polypharmacy. DDI was performed using a drug interaction checker software (www.drugs.com database).6 WHO defines polypharmacy as routine usage of 5 to 8 drugs and excessive polypharmacy as intake of 10 or more drugs.10
The collected data were analyzed with the help of WHO core prescribing indicators such as:9
Results
A total of 600 prescriptions were analyzed. All the prescriptions had demographic details such as hospital ID, name, age, gender, and address with a male predominance of around 324 (54%). The average age group ranged from 7 years to 76 years.
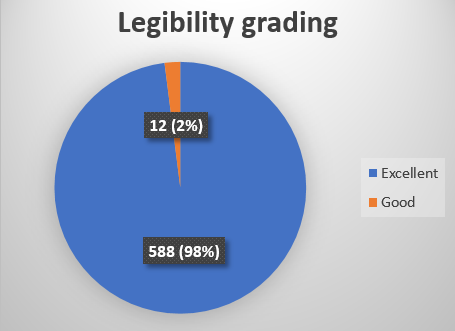
The details about the prescriber’s information such as consultant name, registration number of consultant, date, and signature were shown in Figure 1.
Figure 1
Information about the prescriber available in the prescriptions. The values are expressed as n (%)
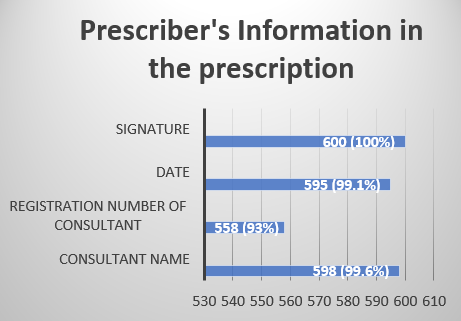
All the prescriptions were assessed for legibility and the grading is shown in Figure 2.
Polypharmacy was encountered in 50 (8.3%) prescriptions along with the common drug-drug interactions which were dizziness, and irregular heart rhythm or QTc prolongation, especially in patients with pre-existing cardiac problems. Drug prescription as per the approval list was followed in all the prescriptions and none of the prescriptions were encountered for therapeutic duplication.
All 1633 drugs were prescribed by the National List of Essential Medicines. The WHO core prescribing indicators were implemented in the analysis of all the prescriptions and are shown in Table 1.
Table 1
WHO core prescribing indicators
Discussion
In developing countries, prescription plays an important role in connecting and conveying medical information between the doctor and the patient. Providing appropriate medicine to the right person with the right dosage and duration stays the ultimate goal of medical practitioners. To assess such aspects, the prescription audit works as a voice to bring out the medical, social, and economical hindrances that are being faced. This helps the health administrators to take strong decisions and to create new policies for the healthcare professionals, and manufacturers. Thereby, a prescription audit helps to improve the overall outcome and the quality of the prescription which gives a way for the medical system to move forward which eventually reflects on the patient’s well-being.
In our study, all the prescriptions contained general patient information details such as name, age, gender, and hospital identification number. This is because of the practice of taking printed stickers at the time of registration itself which are later used to label the patient’s prescription and also during the time of their upcoming visits. Similar findings were also seen in a study done by Ahsan M et al. wherein the reason was due to the practice of printed stickers.11 Following this method of using stickers as a routine practice act as an added advantage to the prescriber for easy identification of the patient thereby improving the quality of the prescription and also serves as a record where retrospective information about the patient can be easily retrieved.
In this study, regarding the prescriber’s information part, the prescription was lagging in the registration number of the prescriber where only 558 (93%) prescriptions had the details about the prescriber’s registration number. A well-maintained prescriber’s information helps the patient with an easy approach to the same doctors during their regular visits and also serves as proof in case of any medicolegal issues.12 The legibility of prescription writing (shown in Figure 2) was well maintained with an excellent grading in 588 (98%) prescriptions. Maintaining good legibility is one of the key factors since they help to avoid confusion and give a clear view of the medication to the patient as well as to the pharmacist.13 The practice of integrated use of the well-kept prescriber’s information along with good legibility of the prescription adds an advantage by acting as a mode of communication between the doctor and the pharmacist which helps in the flawless dispensing of the medications. Furthermore, it can be simplified and improved by adapting to alternative strategies such as using a stamp with the prescriber’s information or switching to electronic devices in the future helps to overcome these minor errors in the prescription.14
The percentage of drugs prescribed in generic names in our study was 99%, wherein compared to a study done in the psychiatry department of a tertiary care hospital in North India which revealed that 85% of drugs were prescribed in generic names.15 Another study done in a rural hospital in Delhi showed that 85.8% of the drugs were prescribed in generic names.16 These studies show the line of increase in the usage of generic names is more prevalent nowadays. Certain initiatives like “Policy Options for Promoting the Use of Generic Medicines in Low- and Middle-income Countries” were taken in the year 2016 to improve the usage of generic prescriptions and educational interventions to promote knowledge about generic medicines and to trust in their qualities, especially in low and middle-income countries.17 In 2018, the Minutes of the 81st meeting of the drugs technical advisory board of India recommended pharmacies have a separate rack displaying a signboard with the word “GENERIC MEDICINES ARE ALSO AVAILABLE” in both English and regional language.18 Using such sign boards helps the patient to know the availability of medication at an affordable range. And among health care professionals, they also help to increase the habit of prescribing generic names compared to the brand name.
This study also revealed a very lower percentage (0.5%) of usage of drugs in the form of injections. Such low usage of injection was also utilized only during an emergency such as anxiety. WHO also recommends the optimal usage of injection with a value range between 13.4 to 24.1%.9 Middle-aged were the most common age group of people seeking psychiatric support whereas schizophrenia, depression, and anxiety was the most prevalent diagnosis. Similar findings were also found in the previous studies done by Aggarwal M et al.15
In our study, the average number of drugs per encounter (expressed in Table 1) was around 4.2 ± 2.5 which was very much closer to the WHO range of polypharmacy. This is mainly seen to rule out the chances of drug-drug interaction since polypharmacy is one of the leading causes. Similar findings were also found in the previous studies done by Abidi A et al.13 They also contribute to other burdens like poor patient compliance, medication error, adverse drug reaction, and an increase in the cost of health care which is eventually reflected in the national health budget. The commonly encountered drug-drug interactions in our study were dizziness followed by irregular heart rhythm or QT prolongation which was present in 85 (14%) and 19 (3%) prescriptions respectively. The cause of the above drug-drug interactions was seen in the drug combinations such as Lorazepam + Haloperidol + Trihexyphenidyl, Lorazepam+ Risperidone, and Venlafaxine + Olanzapine, Lithium + Quetiapine respectively. A literature review done by Fulton MM et has concluded that the risk of DDI increases as the number of drug combinations increases. The event of an adverse drug reaction can rise up to 13%, 58%, and 82% with two, five, and seven or more medication combinations respectively.19 Usage of psychiatric medication in recent days has increased and most of the time they receive a high complex medication.20 Metabolic disorders like hypertension, diabetes, and hyperlipidemia are common comorbid conditions that are highly exhibited along with psychiatric illness and are the reason behind giving priority to DDI in these patients.21, 22 These DDIs mainly occur due to modifications in the drug's pharmacokinetics or pharmacodynamics characteristics, especially with the addition of a drug regimen that either leads to adverse drug reactions or attenuates the drug efficacy.23, 24 Drug absorption, distribution, metabolism, and elimination are the pharmacokinetic mechanism that can be modified by DDIs due to the usage of additional drugs, which can increase or decrease the serum concentration of the drug.25 P- glycoprotein (P-gp) also known as Multidrug-resistant protein 1 (MDR1) is an adenosine triphosphate (ATP) binding cassette subfamily B membrane 1 transporter (ABCB1) is mainly involved in the transport of drugs into the intestinal lumen.26 Drug classes like calcium channel blockers (eg. Verapamil), a macrolide antibiotic (eg. Clarithromycin), etc are a few examples of P-gp inhibitors or its inducers like rifampicin ultimately lead to the development of potential risk for adverse effects due to the modifications in the P-gp transport.27 Since DDI is a preventable medical problem along with one of the common reasons for developing adverse drug reactions and hospitalization, a high caution should be maintained in prescribing the drugs especially elderly group as they are more exposed to multidrug regimens.28 Sedation or dizziness, QT interval prolongation, extrapyramidal symptoms, seizures, etc are the frequently encountered pharmacodynamic DDIs, which were positively correlated in our study.29, 30, 31
Conclusion
This study highlights the importance of regular prescription auditing which not only helps to improve the overall quality of prescription writing patterns but also helps to provide a piece of updated knowledge on the newer drugs, their action, the prevalence of drug-drug interactions, and other common errors which take place in the prescription writing part among health care professionals. As well, they also provide an idea to improve the overall quality of prescriptions. A periodical training program on prescription writing especially using the WHO core prescribing indicators helps to pave a better way for understanding and to know the importance of prescription writing among healthcare professionals which ultimately leads to a better health care system for the community. Also, a detailed history collection about the patient’s comorbid conditions and concomitant drugs can help to overcome unwanted drug interactions.